Research
We seek to understand the neural basis for specific signs and symptoms of brain network disorders, including Parkinson’s disease, isolated dystonia, essential tremor, and Huntington’s disease. Part of our effort is directed to identifying neural correlates of nonmotor symptoms, such as anxiety and depression, in addition to motor signs.
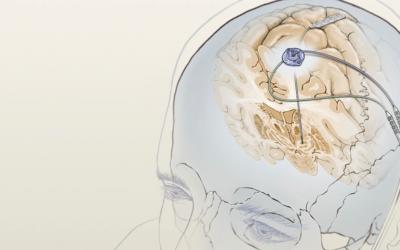
The general approach involves combined cortical and basal ganglia recording in humans. This research effort is complementary to our existing high-volume clinical program, in which approximately 80 new patients per year undergo placement of new deep brain stimulator (DBS) electrodes. Data gathered are used to confirm, refute, or expand upon existing models of basal ganglia and cortical function and dysfunction, to provide a better understanding of the mechanism of action of brain stimulation, and to improve the efficacy of DBS.
Specific Questions Addressed:
1. What brain circuit abnormalities underly specific motor and nonmotor features of movement disorders?
2. How do therapeutic interventions such as DBS normalize activity in the basal ganglia-thalamocortical network?
3. Can the efficacy and adverse effect profile of DBS be improved by incorporated feedback control? Can cortical signals be used to drive adaptive DBS?
Technical Approaches
Acute intraoperative recording of cortical and basal ganglia local field potentials
During surgery for implantation of permanent DBS leads, temporary cortical strip electrodes (electrocorticography, ECoG) are introduced into the subdural space via the standard surgical exposure used for DBS implantation. Basal ganglia and cortical LFPs are recorded at rest, during computer-controlled movement tasks, and during acute therapeutic stimulation. Intraoperative CT is used in conjunction with structural MRI to accurately localize recording sites, and diffusion tensor imaging acquired preoperatively may be used to relate cortical findings to the anatomy of specific fiber tracts.
Interictal electrocorticography in patients undergoing invasive video-ECoG monitoring
In human studies that involve placement of invasive electrodes, true normal control data are not available. However, ECoG data recorded in epilepsy patients, from cortical areas not involved with the epileptic focus, can be considered as a "control" group and be compared to subjects with movement disorders to provide insight into those patterns of brain activity that are specific to subjects with basal ganglia disease.
Chronic invasive brain recording
We are able to record multisite neural signals (LFPs and electrocorticography) from permanently implanted devices that both deliver therapeutic stimulation and sense neural signals. Signals that are sensed by these “bidirectional” neural interfaces may be stored on the device for later noninvasive downloading, or wirelessly streamed continuously to an external computer for many hours. Data may be collected during computer-controlled task paradigms, or during normal activities of daily living in a patient’s home. Implantable sensing devices we use include the investigational neural interface Summit RC+S (Medtronic), since it first became available in October 2018, and the Percept (Medtronic) neural interface, the first commercially available bidirectional interface for movement disorders and psychiatric disorders, since its US release in July 2020.
Noninvasive electrophysiological analyses
This type of study uses scalp electroencephalography.